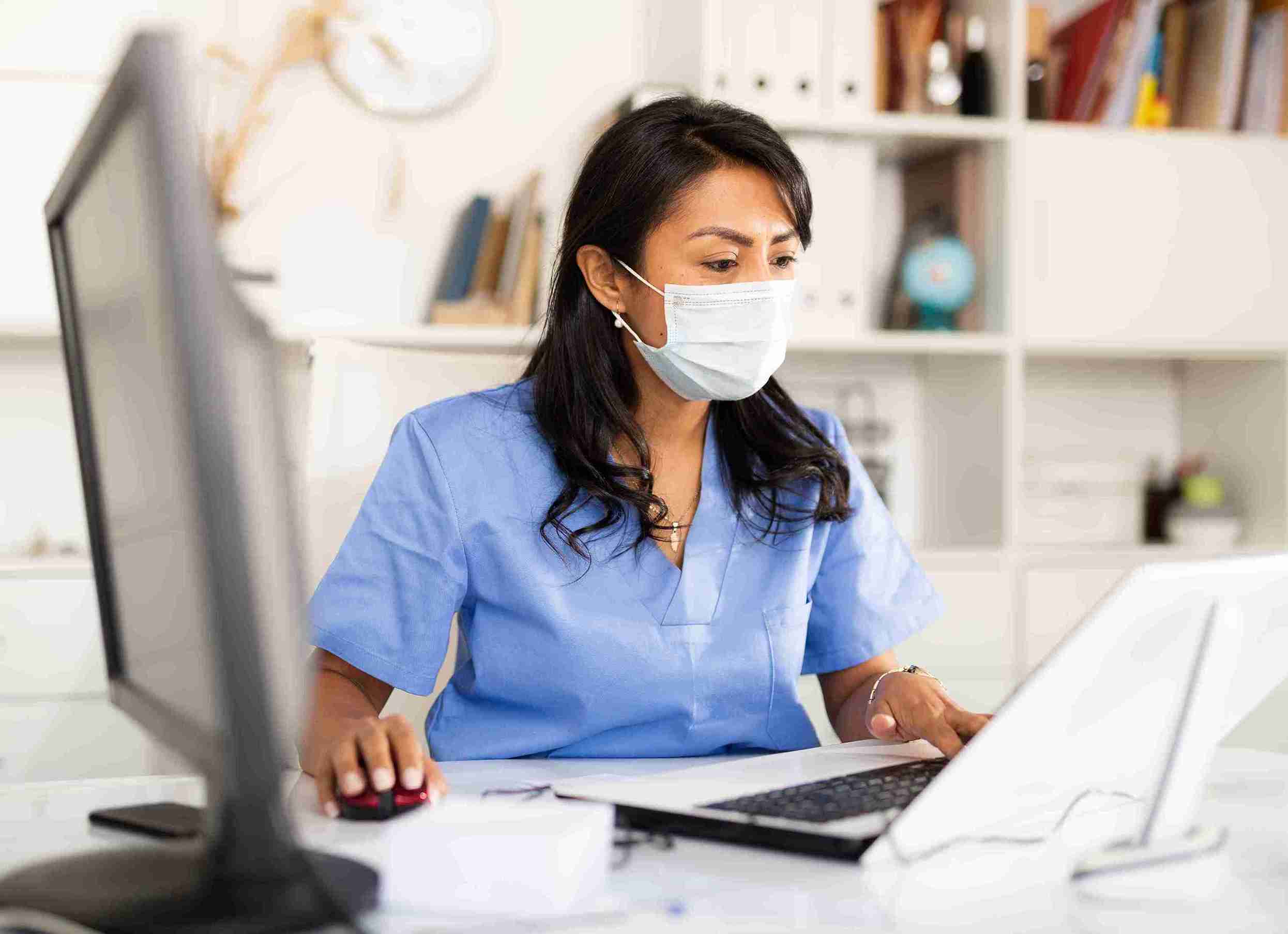
Like most businesses, the early days and weeks of the COVID-19 outbreak had a significant effect on payer organizations. They were caught off-guard by the lockdown mandates and changes that needed to be made to help protect the health of their employees, including the shift to a remote workforce. Without the infrastructure to effectively support a virtual team, payers greatly scaled back their staffing as they worked to build such an infrastructure.
This disruption in payer operations and staffing was felt by ASCs and other healthcare organizations. Claims and appeals processing stalled. Customer support services — which generally weren't all that good before the pandemic — were diminished further. One of the ways most surgery centers were affected by these developments was that they typically saw their accounts receivable (A/R) increase, sometimes significantly.
Now that we're about 18 months into the pandemic, one would have expected that payer operations would largely be back to some semblance of normalcy. The past year and a half should have been enough time for payers to implement the processes and increase their workforce to function at least close to how they operated before the public health emergency. And yet, as we're finding, that's not the case for many payers.
Since ASCs must continue to work with payers to get paid for covered procedures, we must play the cards we've been dealt. Fortunately, there are some ways that we can better navigate the payer challenges we're currently facing and will likely continue facing for some time.
Below I share five quick tips that may help you overcome these barriers to getting paid. For additional guidance, I invite you to register for my upcoming webinar, "Improving A/R Management: How to Turn 'Accounts Receivable' Into 'Accounts Closed,'" which I'll be co-presenting with Jessica Nelson, vice president of revenue cycle services for SIS, on September 30 at 3:00 ET. You can register here.
Here are five tips that I hope will help you!
1. Get documentation completed fast
With the delays we're experiencing with payers, it's even more important for surgeons to complete their documentation quickly so you can send bills out as soon as possible. Delays in documentation completion will contribute to rising days in A/R and even longer waits for payment.
2. Leverage payer portals
Bad news: There's no magic solution for reaching payers.
Good news: We're seeing a growing number of payers with better portals that allow us to learn the status of claims or upload additional information. For example, if a payer denies a claim because processing of the claim requires more information, instead of needing to send that information through snail mail, which is even slower these days, we can often upload that information through a portal.
The more we can use tools like portals to support submission and payment of claims, the more time we'll have for more challenging claims, such as those for workers' compensation.
3. Use clearinghouse's electronic solutions
Speaking of workers' compensation, trying to reach and speak with a workers' comp payer representative is typically even more difficult than reaching a commercial payer. It can be a nightmare of constant follow-up. Even if you get ahold of somebody, the standard answer you will likely receive when asking about the status of a claim is that it's "still in processing" and you should "call back in 30 days."
Fortunately, clearinghouses are increasingly implementing their own electronic solutions that you should be using whenever possible to submit claims and upload supporting documentation like operative reports and medical notes. In addition, you can create custom edits for each of your payers that may help meet payer requirements, thus reducing rejections and denials.
4. Separate payers for A/R management
When measuring days in A/R, it's not unusual to see an ASC including all its payers in that figure. The problem with doing so is that a few payers and just a few claims can greatly skew this key performance indicator (KPI). Consider that workers' compensation and personal injury protection claims, for example, can take many, many months — sometimes even a few years — to be processed. If these claims are included in your days in A/R KPI, the figure will likely be much higher than if they were segmented out.
That's what you should consider doing. Measure the days in A/R for Medicare, commercial payers, and these outliers separately. This will allow you to better monitor and measure the A/R days of each payer type and more quickly identify when problems begin to develop.
5. Go above the payers
When you've exhausted your efforts to reach payers for claims or appeals status updates, consider reaching out to the insurance commissioner in your state and asking what your next recourse should be to receive payment. Be prepared to share details of your payer outreach efforts, including frequency, method of attempted communication, and any responses.
Improving A/R Management: How to Turn "Accounts Receivable" Into "Accounts Closed "
Reminder to please join me and Jessica Nelson on September 30 at 3:00 ET for what I can assure you will be a terrific webinar full of valuable guidance and insight. If you can't attend the live program, please register anyway so you can be notified when the recording is available. And if you're CASC certified, attending the webinar or watching the recording can earn you 1 hour of AEU. Register today!