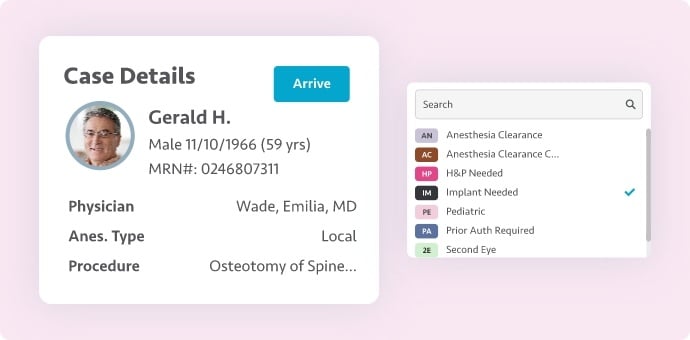
A staggering number of ambulatory surgery centers (ASCs) are not aware of the use they can make of the data found in their electronic medical record (EMR) solution. This information, which is already available at their fingertips, can provide help to improve clinical and financial operations. SIS’ Director of Analytics, Amit Jiwani, hosted a webinar presentation last month to help guide ASC staff on how to best attach value to their data and ultimately improve their operations.
The data you can gather with an EMR begins when a patient’s need for surgery arises and ends after their postop recovery. There are key metrics that can be measured throughout each touchpoint and once you know what you are looking for, you can start strategizing for ways to make improvements. Here are a few key metrics to keep in mind throughout the surgical process:
- Prior to Day of Surgery
You want to make sure you are tracking cancellation rates prior to the day of surgery, but it is also important to factor in the cause of those cancellations when collecting your data. Was the case cancelled due to the patient, the surgeon, or complications at the center? How does the patient education material that was (or wasn’t) provided correlate to your patient cancellation rates? How about the percentage of patients that completed their preadmission paperwork prior to the appointment time? These are all things to consider when drilling down into your cancellation metrics prior to the day of surgery. When you start to see patterns emerge, you can then make formal plans to decrease that cancellation percentage.
- Arrival to Preop
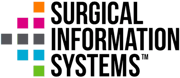
Unfortunately, cancellations can also occur on the day of surgery, and these will need to be evaluated the same way we did prior to day of surgery. It is also important to look at patient wait times. How long was your patient in the waiting room from the time they arrived until their clinical care began? What percentage of their history & physical and/or consents were completed when they arrived versus before the day of surgery?
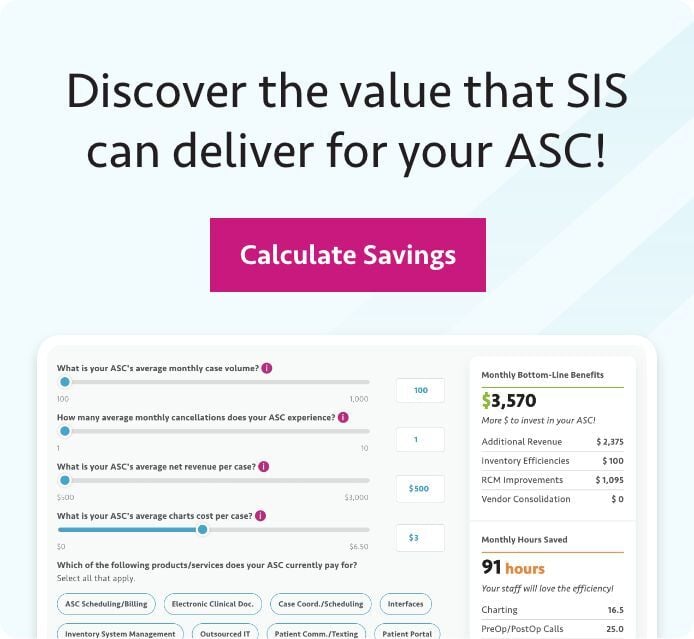
- Preop to Intraop
So, your patient has arrived and checked in, and now they have entered the preop phase. What do you need to look out for? What is the average turnover time (in minutes) for each operating room? What is the average time it takes from the patient’s arrival to the room to when incision begins? Do these averages depend on the surgeon or the procedure being administered? If your operating rooms are delayed and running late, what are the common causes of said delay? Was the procedure scheduled accurately by the front office staff?
- Intraop to Recovery
Finally, it is time to evaluate what is occurring in your recovery rooms. You will want to look at the post-anesthesia care unit (PACU) metrics and determine what the average number of PACU hold minutes are. You can compare those numbers among different anesthesia providers and assess any patterns that suggest room for improvement. You can also compare average recovery minutes as they vary between time of day and/or shift changes.
These are just examples, and they certainly do not cover every metric that is available for evaluation, but it’s a good place to start. Having all this data at your fingertips will help you to identify where the variances occur so you can make meaningful improvements.
Collecting the data and then analyzing it are two different things. During the webinar, Amit continued on to show the audience how to take the key metrics outlined above and put them to use by creating a balanced scorecard as a solid starting point for an ASC. To see the presentation in full, and earn 1 hour of AEU credit from BASC, click here.