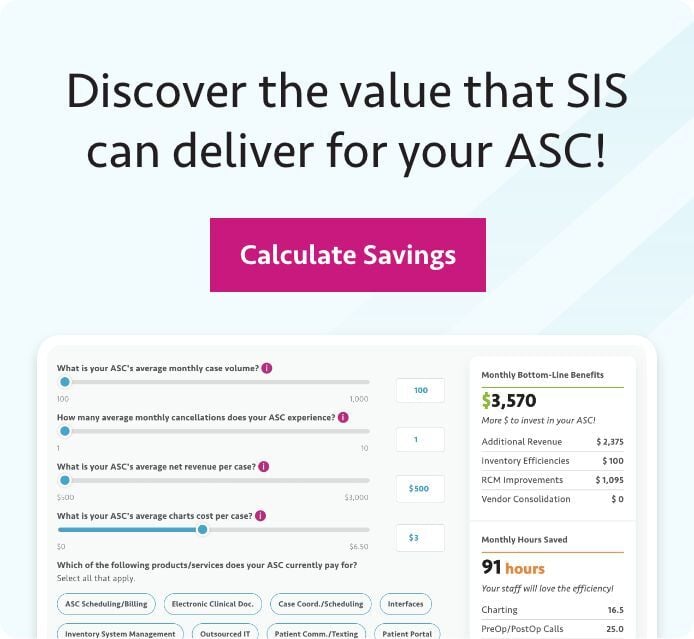
Using effective case costing, an ASC can identify expenses for each procedure performed at their facility, then use that information to maximize revenue.
 It might sound counterintuitive, but an ambulatory surgery center (ASC) performing more cases doesn't always mean it's making more money. There are a few potential ways such an undesirable outcome can occur. For example, suboptimal billing processes that lead to unpaid claims can quickly wipe out potential revenue gains, as can poorly negotiated managed care contracts.
It might sound counterintuitive, but an ambulatory surgery center (ASC) performing more cases doesn't always mean it's making more money. There are a few potential ways such an undesirable outcome can occur. For example, suboptimal billing processes that lead to unpaid claims can quickly wipe out potential revenue gains, as can poorly negotiated managed care contracts.
But even if everything on the revenue cycle management side of things is going well, there's still no guarantee that greater volume will mean a stronger bottom line for an ASC. If the total cost of a procedure exceeds the amount a payer reimburses for the procedure, an ASC will end up in the red for that procedure.
How can ambulatory surgery centers avoid such a scenario? To help ensure the financial success of your ASC, you must make sure you're getting paid enough for your procedure. That means receiving enough reimbursement to cover things like supplies and implants, time spent in the operating room (OR), associated staffing costs, and utilities. And that means you need to determine each of those costs, which brings us to the focus of this blog post: case costing.
Through effective case costing, ASC staff can identify the exact expenses attached to each case performed at their center. With this information, they can determine where adjustments should be made and then take actionable steps to better ensure profitability for cases and procedures and thus maximize revenue.
What to Initially Focus on for Surgery Center Case Costing
Case costing can be daunting, but doing it well is critical to the long-term viability of an ambulatory surgery center. To get started, ASCs may want to focus on the two areas that likely comprise their largest amount of surgery dollars: supplies and overhead. Let's take a closer look at each of these areas.
Supply costs
To gain a better understanding of supply costs, perform a complete inventory audit. Allocate the time necessary to review every item to ensure the correct, detailed product information is logged into your inventory management system. This should include details such as unit of measure, unit price, and dosage per case. "Every item" means literally every single item. That includes something as small as sterile gauze sponges. Doing this detailed work is going to take some time upfront, but the work gets easier when the initial setup is completed.
Once you've finished the complete audit of your surgery center's inventory, load your physician preference cards. These cards should outline all items — once again, every item — your surgeons need for their particular cases, broken out by physician and individual case. Make sure the physician preference cards are as current and accurate as possible. Physician preference cards should be updated as they change. That means clinical staff may need to add items to the card as surgeons alter their preferences or learn about new products. Concurrently, staff must remove items from cards that are no longer used. Failing to perform this due diligence and ongoing updates can lead to incorrect case costing, in addition to other inventory issues that can affect the overall financial health and performance of an ASC.
With a loaded inventory database and updated preference cards, a surgery center now gains the capabilities to cross-reference the information to determine the accurate costs of all supplies for procedures and cases.
Overhead costs
Now let's look at calculating overhead costs by case, which should prove easier than the supply cost calculations, assuming your ambulatory surgery center maintains good records. A simple way to calculate overhead is by determining the cost of the OR per minute. Available medical records should reflect detailed case times so you can determine exactly how long the operating room was in use for cases.
You can calculate the overhead by using this information in conjunction with the profit and loss (P&L) statement for a given month. Begin by subtracting the total cost of medical supplies from the P&L. Then divide the remainder of the operating expenses by the total OR minutes for the same month. The result will be your average OR cost per minute. That average, then multiplied by the number of minutes for an individual case, will yield that case's overhead cost.
Maximizing the Value of ASC Case Costing
Once you have your supplies and overhead data, you can add them together to determine the total cost for each of your cases. Once that's calculated, compare the amount to payer reimbursements for each case and determine empirically if cases are making or losing money for your ambulatory surgery center.
Other discoveries will come out of this valuable ASC case costing data and process. You may notice certain cases and/or specialties are more profitable than others, which can help you prioritize where you may want to work to increase the number of procedures performed at your center. Or through physician preference card analysis, you may notice you're purchasing the same or a very similar product from multiple vendors, which means you're likely not getting the best pricing from any of them. Through case costing analyses of individual surgeons, you can show your ASC's physicians potential opportunities to save money and encourage them to agree to a single vendor. Doing so should allow you to purchase larger volumes from fewer vendors, which should help you secure better prices. For physician owners, consolidating vendors can translate to higher distributions, which should help motivate them to make vendor changes that do not risk decreasing quality of care and outcomes.