Improve the preauthorization process and help strengthen your ASC's collections success using these eight tips.
In the never-ending struggle to receive the deserved reimbursement for procedures performed in your ambulatory surgery center (ASC), it is important to closely — and continually — examine your performance concerning every step of the revenue cycle process. Such proactive efforts are vital to helping ensure prompt, correct payments.
One of these crucial steps begins before the patient even enters the operating room. This step is preauthorization of the patient's procedure. The following are eight tips that can help your ASC improve its preauthorization process.
1. Collect essential information from patients
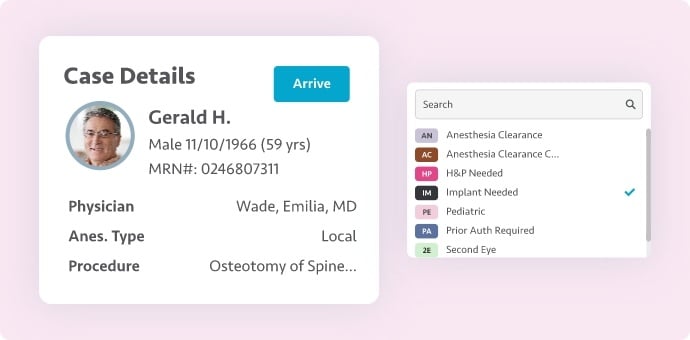
Before contacting a patient's insurance company to request preauthorization, your surgery center's preauthorization specialist should collect essential background information about the patient and their surgery. This includes the patient's name, contact information, date of birth, social security number and insurance details; the name of your performing surgeon; the patient's diagnosis; the procedure type; and the date of surgery.
2. Treat returning patients like new patients
A patient's personal and insurance information can change at any time. Your surgery center's preauthorization specialist should require patients to verify their information with each and every visit to your ASC.
3. Determine payer preauthorization contact preferences
Speak with each of your assigned payer representatives to learn if a payer has a preference for how to receive preauthorization communication (e.g., phone, email, online form/portal). Work to accommodate this request.
4. Carefully time verification of benefits
Verify patient benefits (for primary and any secondary insurance) by reaching out to payers at least 48 hours before the scheduled procedure but no more than two weeks in advance. Patient benefits can undergo frequent changes, so a smaller window of time is preferable.
5. Account for common surgeon practices
It is critical that the CPT codes for planned/documented procedures are preauthorized. However, once the performing physician begins the approved surgery, there may be changes in approach, additional procedures performed based on findings, and/or implants required to complete the procedure.
Your ambulatory surgery center's preauthorization specialist should become familiar with the surgeon's procedures and common changes that may occur and then preauthorize these procedures in addition to the planned procedure. Two examples of common changes that occur are as follows:
- Interlaminar epidural injections (CPT 62323) that are aborted, opting for a transforaminal approach (CPT 64483)
- Planned arthroscopic rotator cuff repair (CPT 29827) is ordered and labral fraying is identified during the planned procedure and is debrided (CPT 29822), or the rotator cuff may need to be converted to an open procedure (CPT 23412)
While some payers will allow a post-procedural update in authorization, many will not, and this can be costly. If there is a high likelihood that a change will occur, be sure the appropriate procedures/codes are provided by the physician and authorized in advance.
6. Stay on top of changing payer preauthorization requirements
It's not unusual for payers to change their authorization requirements. Make sure your surgery center's business office leadership closely monitors correspondence from your payers and identifies any that indicate new or revised rules. Provide information about preauthorization changes to your specialist.
7. Deliver adequate preauthorization training
Help your ASC's preauthorization specialist successfully complete the preauthorization process by allocating appropriate time and resources for training when the specialist joins the business office team. Provide close supervision during initial preauthorization efforts to catch and correct any mistakes and oversights. Establishing good, proper preauthorization practices from the get-go will help reduce the likelihood of mistakes and oversights going forward.
8. Monitor and audit performance
Carefully monitor and audit the performance of your preauthorization specialist. If you identify concerning trends, such as an increase in denied claims due to lack of prior authorization or delayed completion of the preauthorization process, discuss the findings with your specialist and work to address them. Fixing these problems may require training or perhaps additional staff support if the cause of the issue(s) is connected to the specialist's workload.
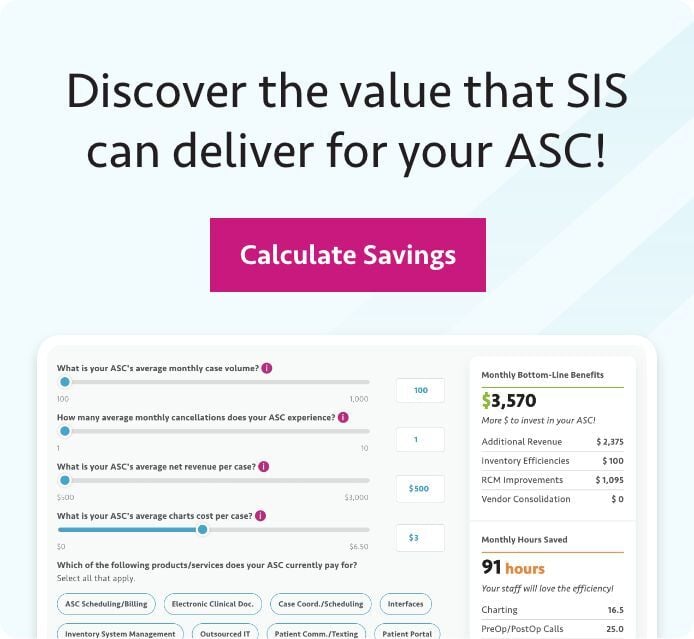
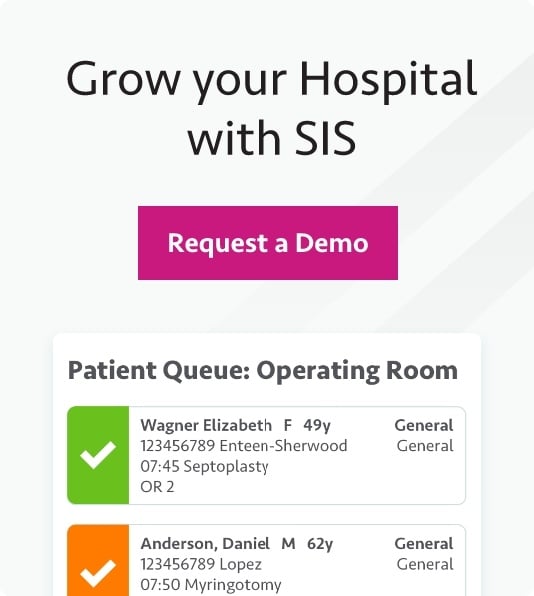
Strengthen Your ASC's Collections Success
A poor preauthorization process is just one of many ways you can hamstring your ambulatory surgery center's efforts to collect what it is owed from payers. If you're looking for expert guidance on other obstacles to receiving deserved payment in your ASC, check out the SIS-hosted complimentary webinar, "Common Obstacles to Getting Paid in an ASC." Watch the on-demand webinar here.
CPT Copyright 2023 American Medical Association. All rights reserved.
CPT® is a registered trademark of the American Medical Association.